CASE STUDY
How HealthJoy’s Proactive Redirection Increased Point Solution Engagement by Over 2.3x
INDUSTRY: ELECTRICAL WORKERS UNION
Benefits programs are often underutilized because members don’t know how or why to use them. In addition, blanket communications aren’t timely or personalized enough to affect employee behavior.
Our union client— that we’ll be exploring below — was well familiar with these challenges. Managing benefits for a population of electrical workers comes with a unique set of challenges. Whether it’s the rigorous nature of the work, which can lead to an increase in musculoskeletal (MSK) related issues like back or joint pain, or addressing the concerns of an on-the-go workforce.
When we began our partnership, our client expressed two main concerns related to their benefits package.
- Members historically underutilized their MSK point solution
- The client wanted to make the most of the benefits they already offered to employees
This is where HealthJoy stepped in to drive results by modernizing their benefits communications and boosting utilization to existing point solutions.

Increasing Point Solution Engagement with Personal Outreach
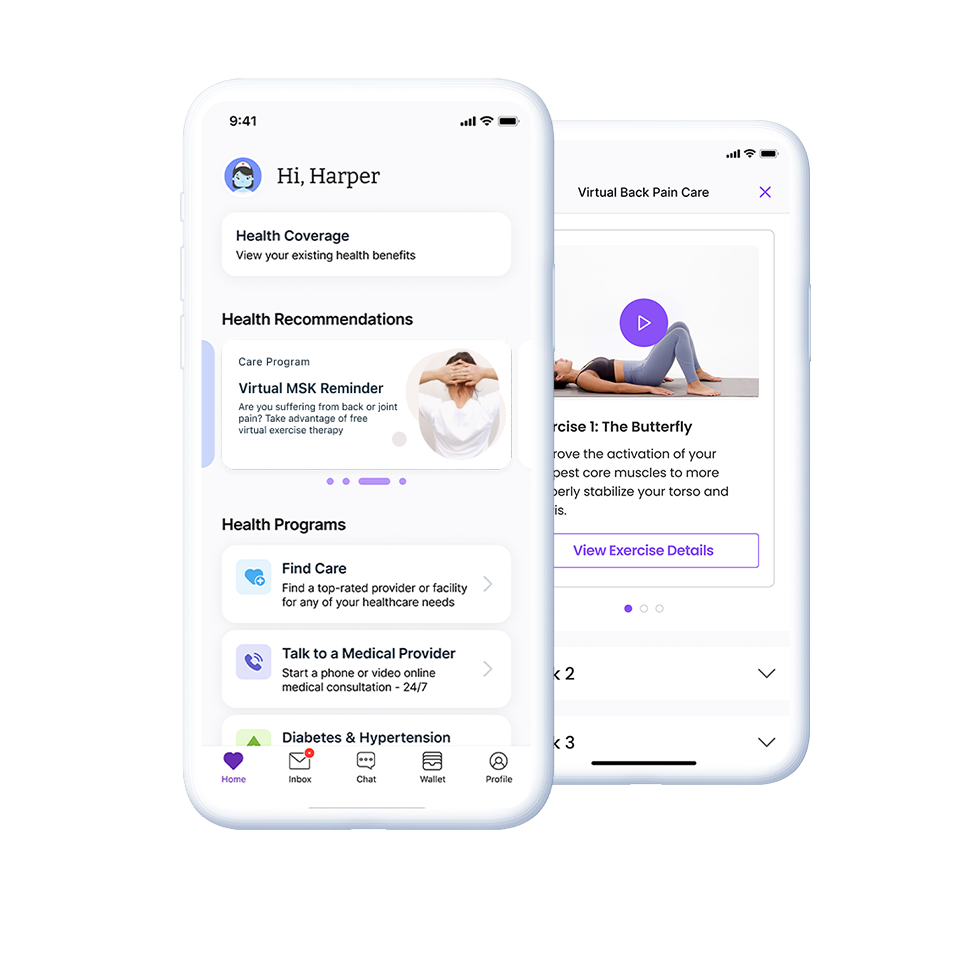
Through HealthJoy’s claims data analytics, clinical steerage, and proactive redirection we can help organizations drive meaningful results — both to our world-class suite of virtual care solutions and to third-party solutions.
Increasing benefits engagement is one of our core competencies and one of the ways we deliver value to our clients. Through our industry-leading tech engagement strategies, we’re already increasing utilization of virtual care. Our technology steps in with the right suggestion at the right time.
To build on this core competency, HealthJoy employs strategies with human connection from clinical coaches trained in behavioral change and motivation. HealthJoy’s outreach efforts provided immediate results to this utility workers union and increased member satisfaction.
The effectiveness of HealthJoy’s personalized outreach, in addition to promoting and redirecting to the client’s MSK solution, led to a significant enrollment boost. Just four months after HealthJoy outreach began, the client saw their utilization rate more than double to 2.3x the rate before HealthJoy stepped in. This increase in utilization rates not only led to significant satisfaction and pain relief for union members, but significant savings for the union. In total, HealthJoy helped to drive $850,368 in MSK savings alone since outreach began.
Utilization rates increased by 2.3x since outreach began, and HealthJoy helped to drive $850,000+ in MSK savings.
Driving Utilization to Cost Containment Solutions
To achieve these results, the HealthJoy team put together a three-step plan to deliver meaningful value.
1. Claims Analysis
HealthJoy collaborated with a third-party MSK point solution vendor to review the client’s claims data and targeted all members who had an MSK claim. Nationally, MSK-related conditions account for $213 billion in annual treatment, care, and lost wages. This makes it the third-highest source of claims spend for 85% of employers. When you combine the financial impact of MSK conditions with the high prevalence — one in two Americans have an MSK condition, according to the World Health Organization — you quickly see how important a strong MSK strategy is. This is especially true for organizations with high populations of industrial workers.
2. Personalized Outreach
HealthJoy’s team of clinical coaches conducted direct phone outreach to over 2,300 members who had an existing MSK claim to drive utilization of the client’s third-party MSK point solution.
3. Follow-Up
Then, after the initial outreach, our coaches followed up with an additional call to increase enrollment.
Then, after the initial outreach, our coaches followed up with an additional call to increase enrollment.
In total, almost 3,400 personal outreaches took place. All members targeted through this outreach were provided with either a personalized enrollment link, or the general enrollment information for the MSK solution.
See How HealthJoy Boosts Engagement and Results
Learn more about how HealthJoy can provide your organization with a top-of-the-line benefits experience and utilization rates that drive game-changing results for your benefits package.
The above case study is one experience of a HealthJoy Client with a subscription to HealthJoy's Enhanced Navigation module. Each Client may have a different experience with HealthJoy and that may vary based on a variety of factors, including the Client's benefit plans, their TPA and/or broker experience, and other HealthJoy modules offered.