Why is benefits engagement crucial for healthcare cost containment?
If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
2 min read
 Dannielle Romoleroux
:
September 24, 2024
Dannielle Romoleroux
:
September 24, 2024
Did you know – six in 10 employees would leave their current company for better health benefits?
Based on that statistic alone – It’s clear benefits are essential to recruiting and retaining the best talent. From the same SureCo 2024 State of Employee Health Benefits report, we know the basics are not going to cut it. Employees want benefits aligned to their wants and needs – from mental health to fertility solutions.
To offer this personalization, employers and their benefits consultants are leveraging various point solutions – designed to reduce healthcare costs and improve health outcomes. point solutions offer tailored intervention and specialized care for a specific health condition (e.g. diabetes, mental health).
The point solution marketplace has skyrocketed in the past several years as more employers adopt them into their strategy. According to a 2023 survey by the National Business Group on Health (NBGH) large employers now manage 15-20 health benefit vendors. This number is up from fewer than five just a few years ago, a clear indication employers want to offer benefits programs tailored to employee needs.
But program expansion comes at a cost – point solution fatigue. A crowded line-up of point solution vendors can weaken employee engagement and make calculating a return on investment challenging. Survey findings from Willis Towers Watson found that 56% of employers experience low point solution engagement and 41% cite a lack of outcomes measurement to assess value.
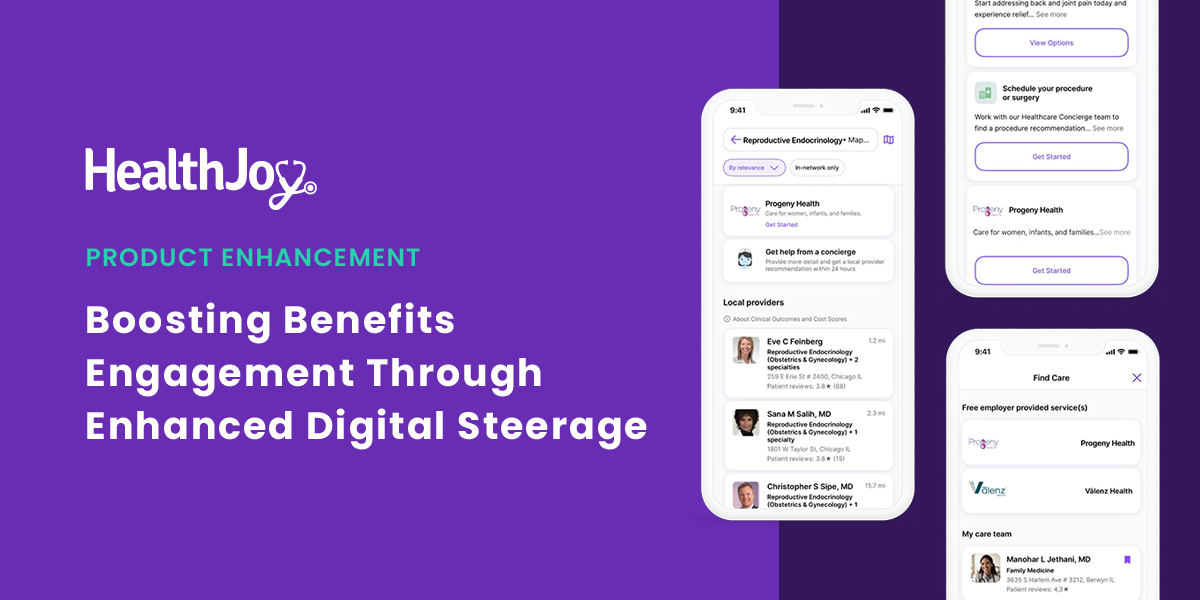
At HealthJoy, we understand that employers and brokers want to continue to offer these benefits solutions and see increased utilization without adding to point solution fatigue. With the new updates in HealthJoy, benefits consultants and employers can proactively surface preferred vendors to employees, at scale, driving utilization and cost savings.
If you’re juggling multiple programs without a centralized platform for employees to access benefits, it’s easy to see how point solution fatigue arises. With a care navigation platform, you can eliminate the clutter of communicating several different benefits at once – streamlining the benefits experience for your employees.
It’s clear the number of point solutions has exploded. At HealthJoy, we know our clients and partners have worked hard to build benefit strategies that best fit their population’s needs. As a result, each client has a unique set of preferred vendors. With our latest release, HealthJoy seamlessly connects your third-party vendors – starting with a list of 50 vendors across EAP, fertility, and surgical – all within one digital experience.
Programs still go underutilized even when the perfect point solution lineup is in place. As an employee, it’s impossible to remember everything you have access to in the moment you need it most. That’s where we come in. With our latest release, we surface your preferred vendors to employees when they search for care. Searching for a reproductive endocrinologist? We’ll highlight your fertility vendor. Trying to schedule a back surgery consultation? We’ll surface your preferred surgical solution.
When the responsibility to drive awareness shifts to a care navigation platform – like HealthJoy, employers can scale engagement with technology and automation. We improve the utilization of your point solutions and drive the return on investment.
During the beta period of this feature, we collaborated with a partner with a population of 65,000+ members to increase utilization to their third–party surgical solution. HealthJoy drove 31% of total utilization and 43% of the partner’s total cost savings for the third-party surgical solution.
It’s clear better benefits engagement leads to improved utilization resulting in cost savings for employers and employees alike.
We’re continuing to invest in supporting additional third-party vendors, and we’d love to hear from you! If you’re new to HealthJoy or interested in implementing a benefits navigation platform, get in touch with a team member to learn more. Connect with your HealthJoy contact or take a quick tour to learn how to make the most of your benefits navigation platform.

If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.

While it may sound obvious, communication is critical to nearly everything we embark on. Strengthening communication strengthens everything:...
Companies are losing the battle against rising healthcare costs without healthcare guidance. Costs are continuing their steady climb with annual...