Stop Managing by Autopsy: Why You Need Real-Time Attribution
Over the course of this series, we have argued that the benefits industry is undergoing a structural shift. We’ve explored the failure of analog...
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
4 min read
 Justin Holland
:
September 25, 2025
Justin Holland
:
September 25, 2025
.png)
The conversation around weight loss has been fundamentally changed by a class of medications known as GLP-1s, with brand names like Ozempic and Wegovy becoming household words. These drugs have delivered life-changing results for many, but their meteoric rise has been met with two significant hurdles: persistent supply shortages and staggering costs, often exceeding $1,000 per month.
For many, the solution came from compounding pharmacies, which provided a legal and affordable alternative during the FDA-declared shortages. But in early 2025, the FDA announced the shortages were officially over, leaving many employers, brokers, and patients confused and concerned. Does this mean compounded GLP-1s are no longer available?
The short answer is no. Compounded GLP-1s remain a legal and viable option, but the landscape has shifted. For the millions of Americans who have lost employer coverage for these medications or simply cannot afford the brand-name prices, understanding this new terrain is critical.
The primary reason for the confusion is a change in federal law. During the shortage, compounding pharmacies were legally permitted to produce “essential copies” of semaglutide and tirzepatide to ensure patient access. With the shortage now resolved, that broad permission has ended.
However, a different legal pathway remains open, one rooted in the core purpose of compounding: personalized medicine. A licensed pharmacist can still compound a medication if a physician determines, for an individual patient, that a specific change to the drug's formula creates a “significant difference” that is medically necessary.
What qualifies as a “significant difference”?
This shift places the focus squarely on a documented, clinical need for a customized medication. While the desire for a more affordable option is understandable, cost savings alone is not a valid medical justification under the law.
The reality is that as many employers have stopped covering GLP-1s for weight management, a massive affordability gap has emerged. Patients who have seen incredible success are suddenly left without access to the treatments that have profoundly improved their health.
This is where responsible compounding pharmacies and the telehealth platforms that partner with them serve a vital role. They are not simply offering a cheaper product; they are providing a crucial lifeline for patients who would otherwise be forced to abandon their treatment. By working with a physician to identify a legitimate clinical need for a personalized medication, patients can continue their health journey in a way that is both safe and sustainable. For employers, helping employees navigate this system is a powerful value-add, ensuring they have access to safe, effective, and affordable care.
While personalizing medicine offers freedom, it also necessitates due diligence. Consumers must be their own advocates in a market with both reputable providers and bad actors. Because compounded drugs are not individually FDA-approved, the onus is on the consumer to verify the source and quality.
Why an employee should care: 503A vs. 503B pharmacies
When it comes to an injectable medication, understanding where it comes from is paramount. There are two main types of compounding facilities, and the difference directly impacts a patient’s safety and peace of mind.
For an employee, a medication from a 503B facility provides a high degree of confidence in its sterility and consistency. However, this does not mean 503A pharmacies are an unsafe option. The key is an additional layer of verification. This is why working with a partner like CareValidate, which vets its entire network of pharmacies—including 503A facilities—through an additional compliance check protocol, is so important. This rigorous vetting process provides an essential safeguard and is the only way we would recommend using a 503A pharmacy.
Due diligence checklist
1. Ask the right questions: A trustworthy provider will be transparent. Before starting any compounded medication, ask:
2. Verify the pharmacy: Never purchase from an online pharmacy without first verifying its credentials. Use the National Association of Boards of Pharmacy (NABP) Safe Site Search Tool at safe.pharmacy to check if a website is properly licensed and accredited.
3. Watch for red flags: Steer clear of any source that sells medication without requiring a valid prescription, lacks a verifiable U.S. address, or doesn’t have a licensed pharmacist available to answer questions.The end of the GLP-1 shortages has not ended access to compounded alternatives; it has redefined it. For the millions of Americans navigating diabetes and weight management without insurance coverage, these personalized medications remain a critical and legal option. The key is to approach the process with knowledge and caution.
Navigating this complex world alone can be daunting. That’s why at HealthJoy, we’ve partnered with CareValidate to provide a trusted pathway for our members. This partnership is designed to help members and their families navigate the system in the safest way possible. CareValidate provides an essential layer of trust by performing its own compliance checks and thoroughly vetting its network of pharmacies. This ensures that whether a medication comes from a 503A or 503B facility, it meets stringent standards for safety and quality.
By providing this guidance and support, we empower our members to make informed decisions, ensuring that when they seek affordable GLP-1 options, they are guided toward sources that prioritize their health. This gives both employers and their employees peace of mind, knowing they have a trusted partner helping them on their health journey.
Reach out to a HealthJoy expert to learn more about our partnership with CareValidate.

Over the course of this series, we have argued that the benefits industry is undergoing a structural shift. We’ve explored the failure of analog...
The Problem The US healthcare system is confusing, overwhelming, fragmented, and frustrating. For employees, the consequences of this unapproachable...
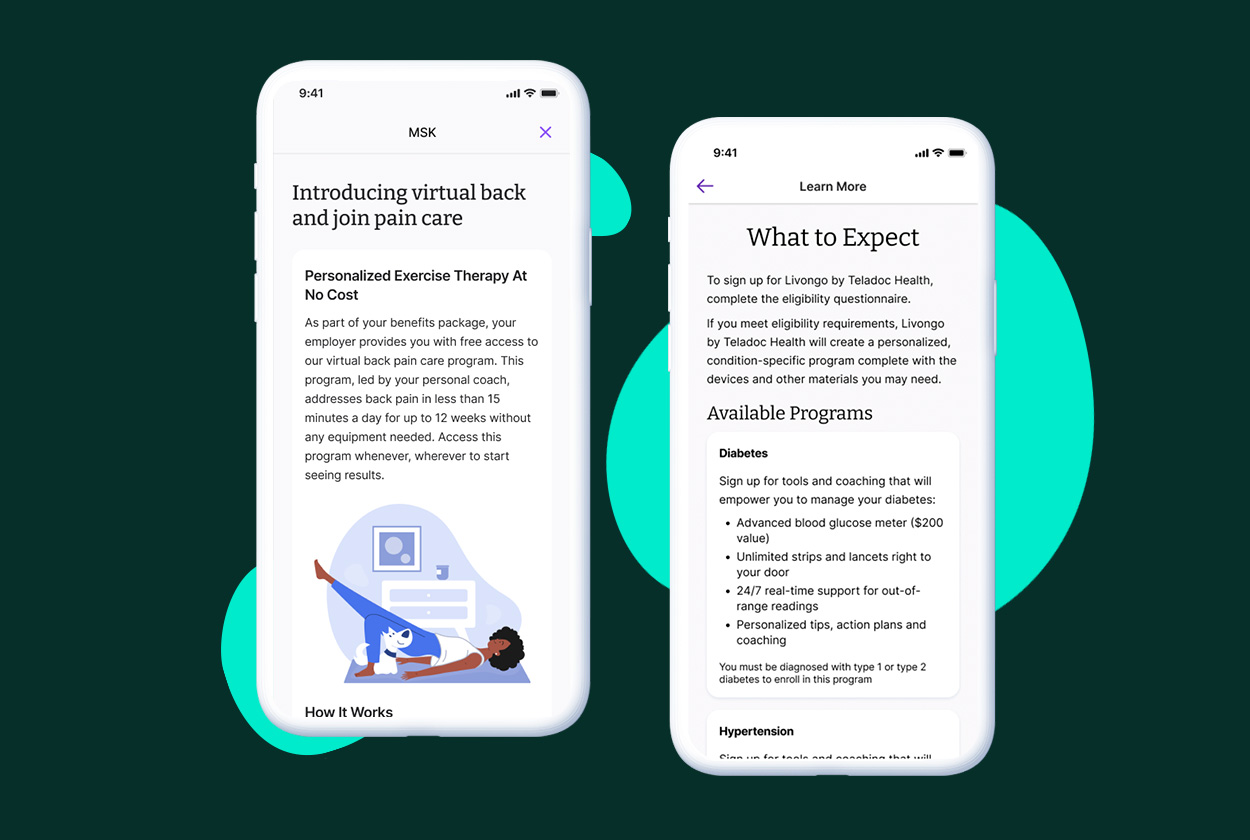
Suffering from a musculoskeletal (MSK) condition can make it feel like you’re on the sidelines in your own life. This pain can take you away from the...