HealthJoy Accelerates Your Cost-Containment Strategy
Employer healthcare costs climb every year. For individuals, the stakes are perhaps even higher.
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
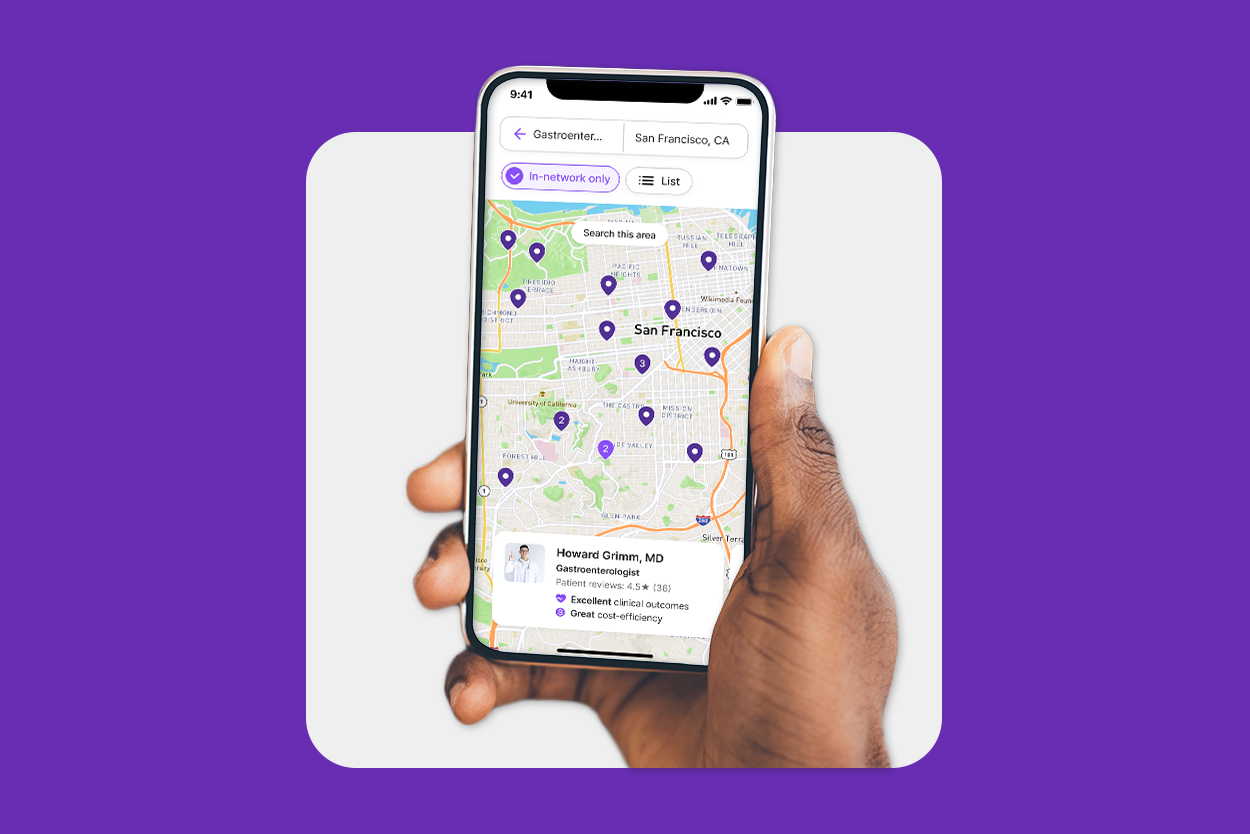
A healthcare navigation platform connects people with the right in-network providers, services and support at the right moment in the employee’s healthcare journey to positively impact the cost of care, while improving health outcomes If you’re unsure whether this type of solution is right for your company, consider whether any of these scenarios apply to your employee population.
Employer healthcare costs seem to be ever-increasing. According to Kaiser Family Foundation (KFF)’s 2024 Employer Health Benefits Survey, the average annual premium rose 6% to $8,951 for single coverage and $25,572 for family coverage in 2024. Comparatively, workers’ wages rose by 4.5% and inflation increased by 3.2% — meaning healthcare costs are still rising faster than both, putting additional pressure on employees’ budgets.
At the same time, enrollment in high-deductible health plans (HDHPs) is increasing year over year, raising the stakes for employee finances. The Bureau of Labor Statistics (BLS) reports that in 2024, 50% of private industry workers were enrolled in High Deductible Health Plans, with the median deductible being $2,750.
Many industry experts are now acknowledging that HDHPs are failing in what they set out to do. One reason is that employees don’t have the knowledge they need to navigate their healthcare plans. Most can’t define the most basic health insurance terms like ‘deductible’ or ‘copay’. And when they choose low-value care, they’re on the hook for unnecessary expenses — and so are you.
If your plan costs are consistently rising, you need a care navigation solution that helps employees find high-value care at the right time.
According to Deel data, Human Resources staff spend as much as 57% of their time on administrative tasks, leaving little time for more strategic tasks.
Employees aren’t in the wrong when they ask benefits questions. The process of finding high-quality, affordable healthcare that’s in-network can be overwhelming for many employees. Healthcare literacy rates are incredibly low; one study found that just 12% of adults have proficient health literacy to navigate the healthcare system, and 36% only have a basic or below basic level of health literacy.
In order to navigate their high-deductible health plans (HDHPs) employees need support. But their HR team is juggling many other priorities, and may not have the capacity to help each individual employee find exactly what they need.
If your HR department is buried in benefits questions, take that as a strong sign you’re in need of a care navigation solution. These programs can surface the best in-network providers to meet your employees needs, so your HR team no longer has to help them find a doctor or direct them to their insurance company’s provider database. A care navigation solution can even prompt them to find savings on everyday healthcare needs, like prescription medications, and use their under-utilized preventive care benefits, like vision and dental screenings.
Best of all, some care navigation solutions – like HealthJoy – come with the expert support of a skilled healthcare concierge team. These healthcare benefit experts are available 24/7, 365 to answer questions and provide steerage suggestions based on your organization’s unique benefits package. They can answer questions and redirect employees on nights, weekends and even holidays – providing an excellent experience for the employee.
Clients share the same response, emphasizing that after implementation, they saw a steep drop in the number of questions routed to HR. With a healthcare navigation solution on hand, HealthJoy client Instructure “never [heard] benefits questions from employees again,” according to Senior Benefits Manager Alli Mauss. “It was like a one-stop-shop; it was like a switch.”
This reduced administrative burden is invaluable for busy HR professionals. HealthJoy is shown to provide HR teams with 142 hours saved per 100 employees each year. That’s a lot of time back that HR professionals can use to focus on other priorities.
According to the U.S. Career Institute, 16% of U.S. based companies are now fully remote. And over a quarter of U.S. households have at least one person who works from home. This is even after many companies opted to enforce return-to-office mandates (RTOs) once the COVID-19 pandemic began to subside. When employees aren’t in the office and are perhaps even spread out geographically, it’s easier for them to feel disconnected to the workplace and what it has to offer. Your HR team might not even be in the same time zone as some employees, so being able to give them a central place to go to access any and all benefits information 24/7 is a huge win.
In other words, remote workers need support from their employer to truly thrive in a digital-first workplace that could be located in their living room, closet or spare bedroom. And just as they’ll need better tools to access remote meetings and company documents, they’ll need a new, digital first way to navigate their healthcare, too.
Not only do remote workers need an easy and convenient way to access their benefits, they may also have greater needs for certain health and wellness benefits like virtual primary care or on-demand chat support to make sure they are selecting services within your healthcare plan’s network.
It’s also been proven that remote workers have increased mental healthcare needs.
While remote work might give us more time to focus on taking care of ourselves, it can also lead to isolation and potentially higher-rates of depression. And on top of that, a lack of 1:1, in-person contact can make it more difficult for managers and co-workers to identify signs of mental health concerns and burnout.
A care navigation tool that surfaces resources like your company’s Employee Assistance Program (EAP) or virtual behavioral health can lower barriers to care and help you reach employees, regardless of their geographic location.
Remote workers also need different support during open enrollment.
Managing open enrollment can still be difficult when you are in an office, and adapting to a remote working environment adds a new layer to open enrollment. This challenge is multiplied if you’re rolling out any major health plan design changes, attempting to promote a brand new benefit, or looking to re-engage employees in their benefits broadly.
A care navigation platform shouldn’t offer only the tools employees need to find healthcare – it’s important that the tool you choose can address the things that they truly want from their benefits experience as well. Your employee population can benefit from a robust platform that offers custom communications, personalized recommendations, and a centralized experience can smooth the process of plan changes, increase adoption and utilization of new benefits and offer a way for remote employees to find the human guided support they need to make the most of all their benefits.
In a self-funded insurance plan, an employer assumes more risk than they would on a fully-insured plan.
From a cost-containment perspective, this means it’s even more important that employees know how to access care that meets their needs and their budgets. In short, it makes a strong case for a care navigation solution.
Self-funded employers normally work with a third-party administrator (TPA) to process and adjudicate their employee benefits claims. TPAs have access to a wealth of information that, when paired with the right care navigation solution, can help benefits leaders proactively confront long-term healthcare spend by reducing high-cost claims and improve employee health outcomes.
A care navigation solution that can work directly with your TPA, like HealthJoy, allows for greater collaboration between companies, their TPAs and their employees.
Using pre-certification and claims data accessible only through a TPA partnership, HealthJoy can get ahead of costly healthcare decisions that lead to increased claims and high costs for self-funded employers. Our data shows that high-cost claimants who activate HealthJoy experience 21% lower healthcare spend compared to employees who don’t activate HealthJoy.
According to Allstate, reference-based pricing (RBP) reduces healthcare spend by up to 20%. Reference-based pricing also creates transparency around costs and empowers plan members to make better decisions for their healthcare.
On the other hand, while reference-based pricing can reduce costs for both employer and employee, it can also place an unacceptable burden on employees.
Typically, a health plan provides a list of services, pricing structure and providers who will accept the reference price for each service. But employees must be willing to do the research. When they aren’t well-educated on their specific plan or guided to appropriate providers that will meet their unique needs, the employee is left to pay the difference between the reimbursement maximum and the provider’s charge. This is called balance-billing. Even successful RBP plans can leave employees with more cost-sharing.
Of course, companies on RBP don’t want to sacrifice quality for cost. For any health plan to work, employees will need to be able to locate high-quality providers. The good news is that cost and quality don’t seem to be correlated. The bad news is that finding a provider who balances the two can prove to be tricky.
To maximize success and minimize problems associated with RBP, you need a care navigation solution that will consistently educate, engage and help employees make decisions based on the plan they currently have.
If your company is dealing with any of these scenarios, it might be time to consider rolling out a care navigation solution. With the right combination of automation, personalization and human-guided support, you can empower employees to make the most of their healthcare benefits without sacrificing cost or quality.
Want to learn more about HealthJoy’s care navigation solution? Register for our demo webinar.
Disclaimer: This is an updated version of a blog that was originally posted in February of 2022.

Employer healthcare costs climb every year. For individuals, the stakes are perhaps even higher.

3 min read
For the average adult in the US, spending a third of their lives in the workplace is just a fact. So it’s no wonder the state of employees’...

It’s that time of year again. As the air gets colder and more people cozy up inside, workplaces must grapple with more than just coronavirus...